By Dr. Melissa Mitchell, DC, CFMP
The month of June is a time in which fathers are celebrated, so it is fitting that June is also the time in which we honor men’s health.
A health issue on the forefront of male health is the depletion of testosterone. The litany of symptoms that are associated with low testosterone can be what makes a man feel like less of the man he once was. There are multiple life threatening consequences of low levels of testosterone in combination with other hormonal imbalances and unfortunately, many are unaware of the serious associated health risks.
The primal instinct to not show signs of weakness is oftentimes what causes men to minimize symptoms and can be what prevents them from seeking medical attention. The early recognition of signs and symptoms and appropriate actions can prevent serious health consequences in older age.
Testosterone Function & Imbalance
- Functions of Testosterone²⁻⁴
muscle mass development, bone growth, body and facial hair growth, deepening of the voice, penis and testicle growth, sperm production, sex drive², red blood cell formation³, increased HDL performance⁴ - Symptoms of Low Testosterone¹
low sex drive, erectile dysfunction, gynecomastia (male breasts), decreased body hair, fatigue, loss of muscle strength/mass, increased body fat, infertility, depressed mood, irritability, poor concentration/memory, decreased sense of well-being, decreased hemoglobin/mild anemia, osteoporosis - Causes of Low Testosterone¹
aging, excess estrogen (via enhanced aromatase activity), obesity, metabolic disorders, decreased blood supply to the testes by injury or infection, chemotherapy/radiation, pituitary gland dysfunction, medications (i.e. opioids, steroids, prostate cancer hormones, statins²⁴), alcohol abuse, liver/kidney disease, HIV/AIDS, genetic predisposition, congenital defects, sleep apnea, anabolic steroid use
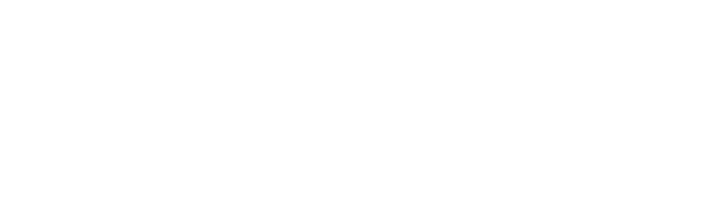
Testosterone Synthesis
Cholesterol begins the process of testosterone production. Cholesterol is converted to pregnenolone which can then be made into either DHEA or progesterone in separate pathways to become testosterone.
As men age, testosterone production naturally decreases. The current medical approach to treating low testosterone is to prescribe testosterone, but there may be other approaches that can prevent the downstream effects that result in low testosterone that may lead to further serious health complications.
Cholesterol is converted to pregnenolone, which can then be made into either DHEA or progesterone in separate pathways, to become testosterone.
The Delicate Balance Between Hormones
The intertwining of androgen/hormone producing pathways makes it easy for unchecked imbalances to occur and can be tricky for some doctors to find where the downstream effects stem from. This exquisite balance is necessary for one to express optimal health given that hormones affect every aspect of human physiology.
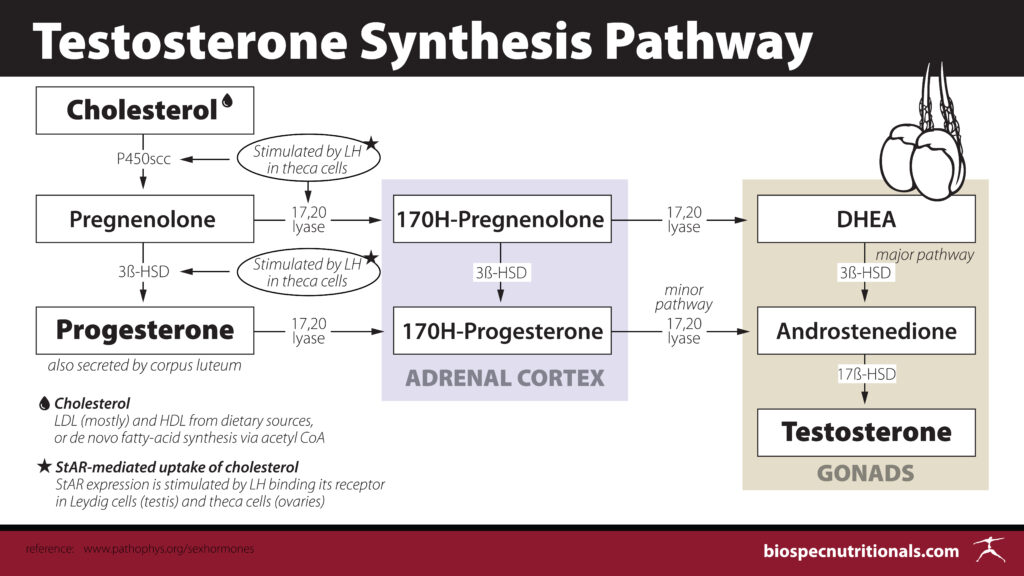
Pregnenolone (Cortisol) Steal
In states of stress, the body will shunt pregnenolone down the pathway to become cortisol. This is a natural process that should occur in acute situations. The theory of cortisol steal states that when chronic stress persists, resources are continuously pulled into the cortisol production pathway and away from the pathways that produce testosterone, estrogen and aldosterone. In this situation, commonly ordered hormone lab values may show low levels of progesterone, DHEA-S, Estrogens and/or Testosterone. Some theorize that stress may reduce the production of DHEA rather than the idea that elevated cortisol “steals” pregnenolone.⁵
When chronic stress persists, the body’s preference to protect cortisol production at the expense of other hormones referred to as Cortisol Steal.
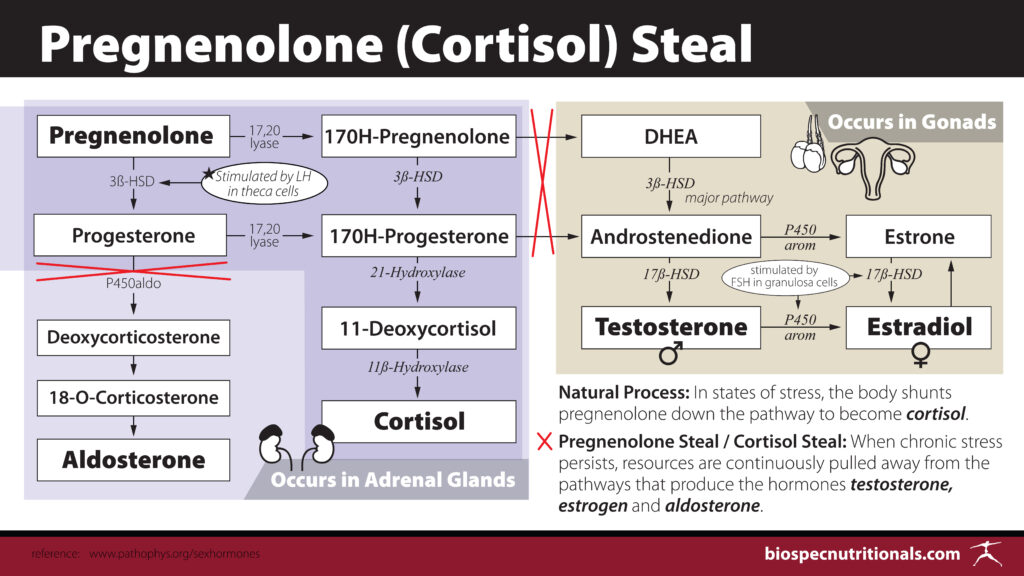
A 24-hour cortisol test will be able to evaluate cortisol production throughout the day, which is far more informative than a one time cortisol test taken at a random time.
The natural levels of cortisol should show an elevation just before rising with a peak early morning and a decline throughout the day. Any shift from this normal flux of cortisol can have detrimental effects on not only hormone production but also immune function, blood sugar regulation and much more. It is imperative to address all sources of stress, both mental and physical, when trying to balance hormone levels.
Enhanced Aromatase Activity: Testosterone to Estrogen Conversion
Androgens can be converted into estrogens (testosterone into estradiol) by the enzyme aromatase. This process known as aromatization functions to maintain the balance between hormones. Naturally, as testosterone production declines in older men, aromatase activity increases, enhancing the conversion of testosterone to estrogen, causing further decline of testosterone levels. Another significant cause of increased aromatase activity is adipose tissue, most notably, abdominal fat. Poor nutrition, weight gain, stress and lack of exercise are also contributors to aromatase activity enhancement. Elevation of estradiol in combination with low testosterone in males can increase the risk of significant health crises such as stroke⁶, cardiovascular events⁷, colon cancer, prostate cancer and male breast cancer. ⁸ ⁹ ¹º
Oftentimes in conventional medicine, testosterone is prescribed to men with low levels without checking estrogens. Men given testosterone replacement may run the risk of converting testosterone to estradiol with elevated aromatase activity which can place them at higher risk for the aforementioned conditions.
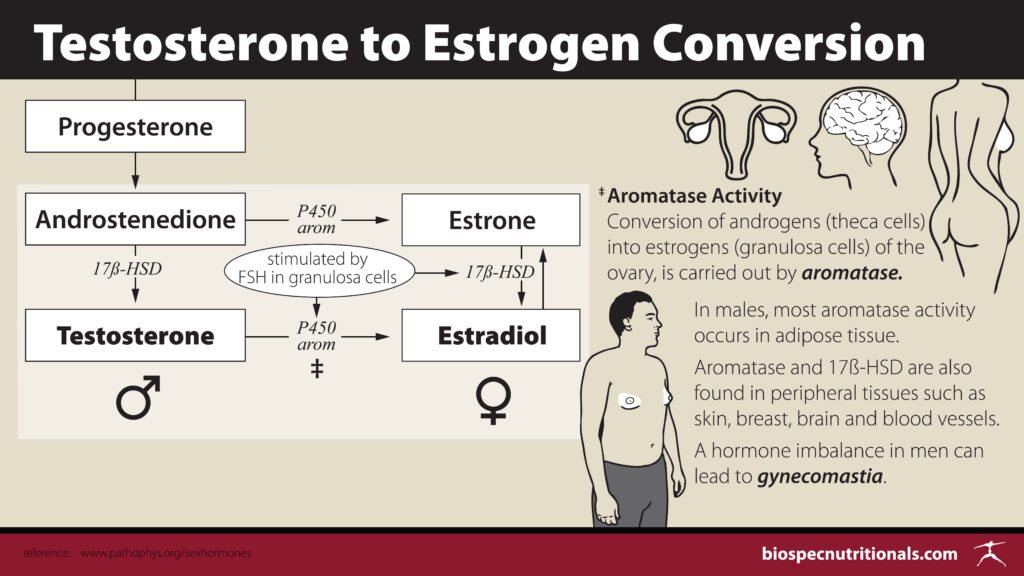
A hormone imbalance in men can lead to gynecomastia.
Low Estrogen
Excess levels of estrogens are a more common occurrence in males, but low estrogens also pose a risk to men’s health. The way in which men synthesize estrogen is through the aromatase enzyme, mostly occurring in adipose tissue. Some men may lack the aromatase enzyme whereas others may have inadequate levels of testosterone to convert to estrogen. Low levels have shown to increase the likelihood of developing osteoporosis and associated bone fractures.¹¹ ¹²
A study published in JAMA found that men with chronic heart failure whose estradiol levels fell outside of the range of 21.80-30.11 pg/mL showed increased rates of mortality. Those in the highest and the lowest quintile of estradiol levels were significantly more at risk.¹³ Perhaps checking estrogen levels in male cardiovascular patients is a huge missing piece in the current mainstream approach to assessing cardiovascular disease risk.
STUDY: HEART FAILURE MORTALITY RATES LINKED TO ESTRADIOL
Factors in Hormone Regulation
The Testosterone and Cholesterol Connection
High Density Lipoprotein (HDL), the “good” cholesterol, is the only lipoprotein that scavenges cholesterol in the blood vessels and tissues and returns it to the liver for processing and removal. Testosterone increases the activity of hepatic lipase, an enzyme that cleaves HDL derived cholesterol and also increases B1 receptor sites in the liver that uptake cholesterol for processing and removal.¹⁴ ¹⁵ The relationship between testosterone and HDL is one that should be further considered by practitioners for the prevention and removal of arterial plaques and for overall cardiovascular health in men.
How Vitamin D Plays a Role
Vitamin D receptors as well as Vitamin D metabolizing enzymes are found throughout the male reproductive system, which includes the Leydig cells that produce testosterone. Because of this, it has been theorized that vitamin D may play a role in the production of hormones and thus studies have been performed to assess the effects of vitamin D supplementation on androgen levels. A provocative study¹⁶ published in 2012 found that 2,069 males who were referred for coronary angiography with low free testosterone or vitamin D had a 60% increased risk of mortality due to non-cardiovascular related causes. If there was a deficiency in both Free T and vitamin D, the risk of death due to a cardiovascular event was 77%. Even worse, those with low levels of both markers had a 133% increased risk in non-cardiovascular related mortality.
Interestingly enough, recent studies have hypothesized that vitamin D supplementation may have positive effects on the production of androgens (testosterone), but current testing models show no apparent connection between the two resulting in unchanged levels of androgens between the two groups of participants.¹⁷ Given that the anatomy/physiology of the male reproductive system is flooded with vitamin D receptors and enzymes, there must be a role that vitamin D plays in hormone production that goes beyond our current understanding or testing methodology. The ubiquitous nature of vitamin D in human health would warrant obtaining optimal levels regardless of the condition(s) being assessed and treated.
Magnesium and Testosterone¹⁹
Often with aging comes muscle wasting/decline of muscle mass which can be linked to not only low testosterone but also low levels of magnesium. Studies have shown a positive response in muscle mass and activity as well as testosterone levels when supplementing with magnesium along with exercise. Animal models have shown a clear improvement in measured physiologic, cytologic, morphologic parameters and cellular architecture of the testes following magnesium supplementation.
The decline in testosterone related to aging, reduced physical activity, poor nutrition and inflammation should be addressed with a focus on magnesium status. Inflammatory cytokines reduce LH production in the pituitary which leads to less output of testosterone and sensitivity to LH secretion. Magnesium helps to control oxidative stress and maintain antioxidant capacity, both significant contributors to inflammation. Dosage of 420mg/day of magnesium is adequate for healthy men. Some studies have seen more improvement when administering 500mg/day.
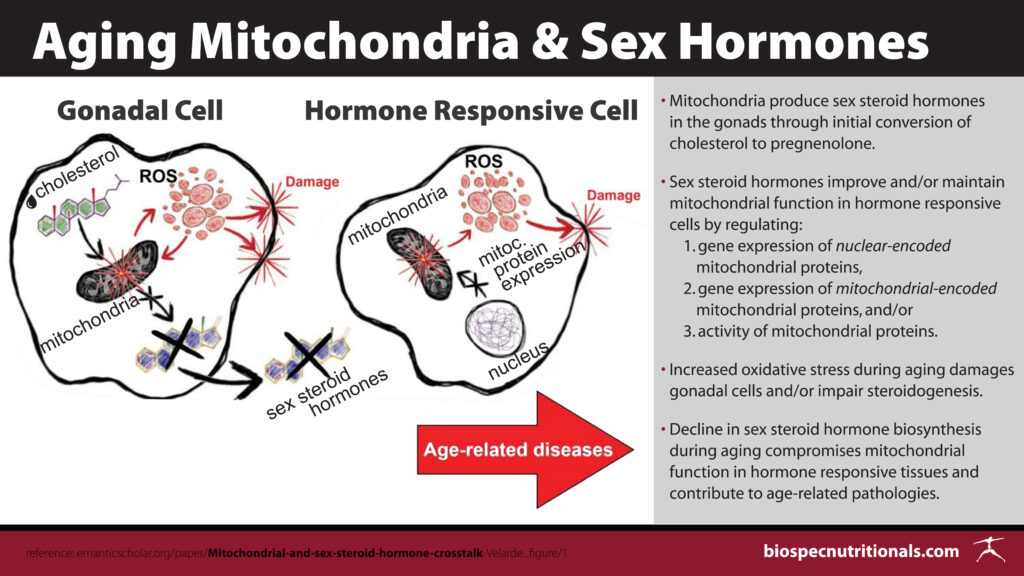
Mitochondria and Sex Hormones²⁰
The mitochondrial membrane is involved in the first, rate limiting step in sex hormone production. Cholesterol passes through the membrane and is converted to pregnenolone which is then transferred out of the mitochondria to be converted into differing sex hormones. The need for a healthy mitochondrial membrane is relevant in the downstream manufacture of adequate testosterone levels. Animal studies have looked at the presence of increased ROS within mitochondria of Leydig cells in older rats compared to younger subjects and in these studies, the elevation of ROS inhibited the production of testosterone.
Inversely, studies have shown the positive impact of sex hormones on the health of mitochondria. Although testosterone and progesterone have been less studied, estrogen has shown to modulate gene expression for mitochondrial function, i.e. mitochondrial respiration, mitochondrial protein synthesis and mitochondrial biogenesis. Sex steroid receptors have been shown to protect mitochondria from damage caused by reactive oxygen species. More investigation needs to be done on the direct effects of testosterone on mitochondria, but our current understanding of the presence of estrogen has shown favorable results in mitochondrial functionality. Men who lack sufficient levels of testosterone necessary to convert to estrogen (low estrogen) may perhaps suffer a negative outcome on mitochondrial function and preservation.
Testosterone, Insulin Sensitivity and Obesity ²⁰ ²¹
Research has found a connection between low levels of testosterone, decreased insulin sensitivity and visceral adipose tissue (abdominal fat) although the connecting factors still remain unclear. There are theories that low testosterone leads to the development of abdominal fat via inability to metabolize triglycerides properly, leading to insulin resistance. What has been seen in animal studies is that castration of male rats leads to the development of insulin resistance and subsequent testosterone supplementation corrects the insulin response.
Some human trials have shown testosterone administration to be beneficial with insulin resistance whereas others have seen no correlation between the two. The correlation was stronger in studies looking at obese men with diabetes. Diabetes can also create microvascular complications which have been associated with low testosterone, low DHEA and elevated estrogen.²² These findings should encourage a healthy lifestyle to avoid the onset of diabetes and obesity, specifically visceral fat, to negate the potential association between low testosterone, insulin resistance and obesity.
Endocrine Disruptors²³
There are numerous compounds, both natural and manmade, that affect the endocrine system and thus interfere with hormone production. These endocrine disruptors are found throughout our environment, in our food, water, household products, hygiene products, furniture, insecticides and medications, to name a few. Some of the more commonly known ECDs are BPA and phthalates found in plastics, perfluoroalkyl substances (PFAS) in industrial products like textiles, furniture upholstery and paper, butylated hydroxyanisole (BHA) a food preservative, and in medications such as ketoconazole, an antifungal, medroxyprogesterone acetate prescribed for abnormal sexuality in males, etomidate a general anesthetic. Even food compounds like resveratrol, flavones and isoflavones have been shown to affect hormone production.
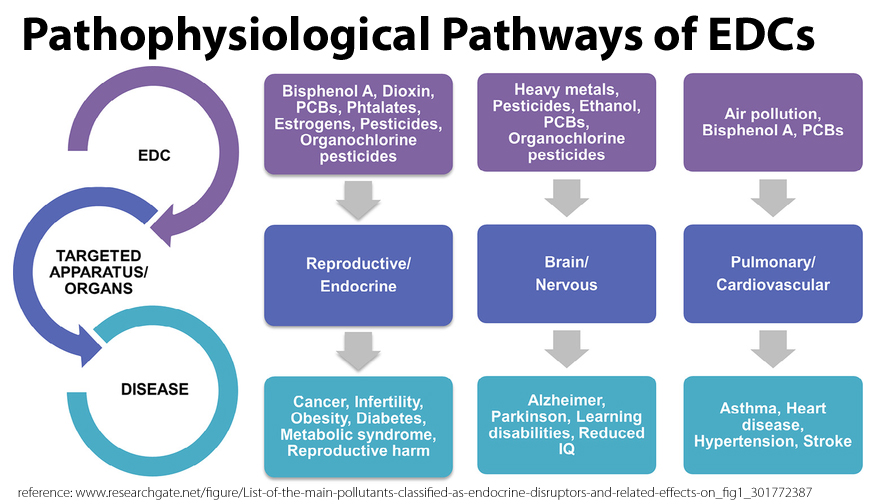
These compounds can cause androgen producing enzyme inhibition (HSD3B), cause disruption in Leydig cell development, can bind to estrogen and androgen receptors acting as estrogens and androgens respectively, inhibit testosterone synthesis and can inhibit androgen production.
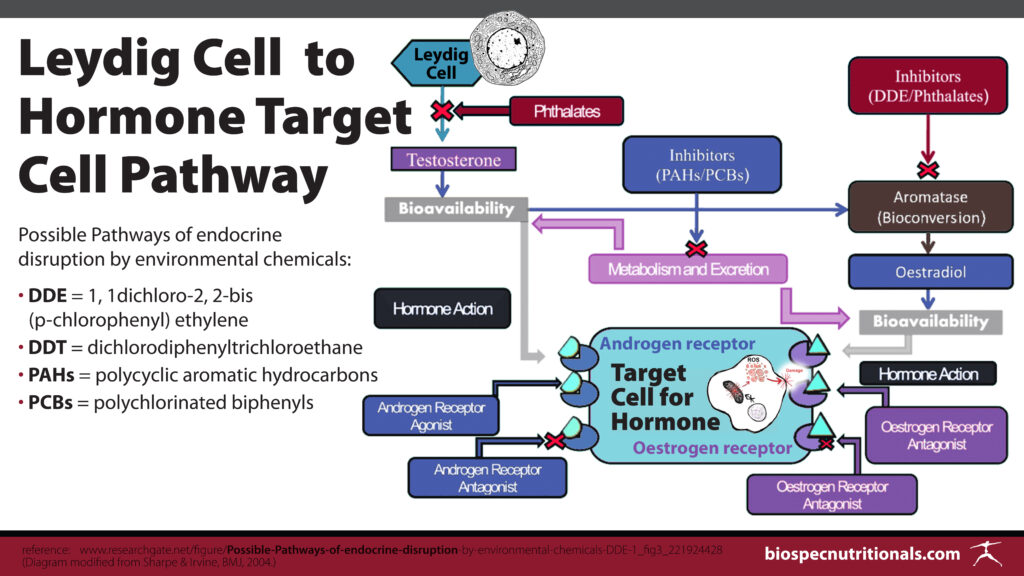
Many of these endocrine disruptors remain in the body for quite some time due to their long half life, all the while, their synergistic effects remain unknown. Many of these compounds have effects within the mitochondria as well, altering mitochondrial function which can be problematic in hormone production as previously stated.
Statins²⁴
A systematic review has shown an association between cholesterol lowering statins and their negative effects on the production of testosterone. Unfortunately, numerous physicians ignore the detrimental effects of low cholesterol with the mere focus on lowering cholesterol levels. Optimal total cholesterol levels are between 150-199 mg/dL. Cholesterol plays a significant role in so much of human physiology and thus it stands to reason that lowering cholesterol levels to an unhealthy range may be detrimental to not only hormone production, but to so many other physiologic processes in the body.
The Copper/Zinc Imbalance²⁵ ²⁶
A 2011 study found that men with elevated copper and low levels of zinc had lower levels of testosterone. Zinc plays a significant role in the activation of testosterone producing Leydig cells. With aging and inflammatory states, mechanisms are set in place to decrease zinc concentrations and elevate copper, altering the repair and maintenance status of an individual, most notably in aging populations. This alteration in the copper to zinc ratio can also play a significant role in the development of cardiovascular disease, malignancy and all-cause mortality. Other contributing factors to the imbalance of these two nutrients are oxidative stress, dietary deficiencies, and elevated insulin levels. A serum/plasma copper to zinc ratio above 2.0 is indicative of an inflammatory state and a zinc deficiency.
Action Steps
PROMOTE HEALTHY TESTOSTERONE LEVELS
1. Reduce cortisol production to reduce the potential cortisol/pregnenolone steal by developing stress coping mechanisms, avoiding stress triggers and/or finding an outlet to release built up negative emotion.Summary & Action Steps
Adaptogenic herbs to negate the effects of stress: ashwagandha, ginseng, rhodiola, astragalus, holy basil, milk thistle, licorice root. Caution is advised with licorice root as it can also have effects on blood pressure. In this case, deglycyrrhized licorice root can help to avoid any potential unwanted effects.
2. Reduce aromatase activity with changes in diet, increased physical activity and reduction of stress. Addressing these lifestyle factors can help with weight loss which is also a contributor to increased aromatase activity.Dietary recommendations : cruciferous vegetables (i.e. broccoli, cabbage, brussel sprouts, kale, arugula, cauliflower, collard greens, turnip, radish); members of the allium family (i.e. garlic, onion, leek, green onion, chive; flavones found in the citrus family, passionflower and chamomile; healthy fats (i.e. coconut oil, raw nuts and seeds, EV olive oil, avocado); fermented foods (i.e. sauerkraut, kimchi, apple cider vinegar).
3. Elevate low estrogen levels to reduce the risk of developing osteoporosis and associated fractures. Increasing the production of testosterone to convert to estrogen via aromatase should be the approach given the concerns in research that lie in the uncertainty of the mental effects of phytoestrogens (specifically genistein found in soy) in male populations. Some studies have shown improvement in cognitive function while others have shown decline with soy/genistein administration.¹⁸
4. Estradiol levels between 21.80-30.11 pg/mL showed to have the best health outcomes for those with cardiovascular disease.
5. Increase low HDL levels with healthy fat consumption and omega-3 supplementation to enhance the antiatheroscelrotic role that testosterone plays in relation to HDL activity and cardiovascular health.
6. Maintain healthy levels of total cholesterol between 150-199 mg/dL for optimal conversion through hormone production pathways.
7. Increase vitamin 25-OH vitamin D levels to a [bare] minimum of 50-60 ng/mL through safe exposure to sunlight, vitamin D3 supplementation and diet.Dietary Sources of Vitamin D: Cod liver oil, wild caught salmon, sardines, mushrooms, egg yolk, beef liver
8. Test serum magnesium levels and supplement accordingly. Adequate levels should be between 0.75–0.95 mmol/L or 1.7–2.5 mg/dL.¹⁹ One particular study found the most improvement in testosterone levels when 500 mg/d¹⁹ was administered to those with low levels.Dietary Sources of Magnesium: Dark leafy greens, nuts, seeds, legumes, avocado, banana, dark chocolate, fatty fish (i.e. salmon mackerel, halibut) and whole grains
9. Maintain mitochondrial integrity to allow for the conversion of cholesterol to progesterone which can then be converted to other sex hormones outside of the mitochondria. Adequate levels of estrogen are needed for mitochondrial protection from reactive oxygen species.
10. Control weight and blood sugar with proper diet and exercise to reduce the role they may play in hormone synthesis.
11. Reduce or eliminate the exposure to endocrine disrupting substances while promoting detoxification and mitochondrial health to eliminate previous toxin exposure stored in body tissues.
12. Maintain a serum copper to zinc ratio below 2.0 with adequate intake of dietary and/or supplemental zinc, reduction in systemic inflammation, insulin stabilization and oxidative stress reduction.
Dietary Sources of Zinc: Oysters, crab, lobster, grass-fed meats, beans, nuts, pumpkin seeds, yogurt and peas
Therapeutic Considerations
ANDRO-XY PLUS
Natural Male Hormone Support
A blend of botanical extracts along with DHEA that have shown to enhance testosterone production in males, reduce estrogen production, reduce the effects of elevated cortisol production, enhance libido, increase energy and improve sexual function.
BIO D/K PLUS
In aging individuals, vitamin D synthesis is significantly reduced, lowering the availability for the use throughout the male reproductive system. A combination of both vitamin D and vitamin K has shown to improve bone mineral density, cardiovascular health, blood sugar stabilization and insulin sensitivity compared to vitamin D supplementation alone.
» Bio D/K Plus (oil-emulsified DR veggie cap)
MAG GLYCINATE 450
A highly absorbable form or magnesium with a daily dosage of 113% of the recommended daily value. Magnesium supports cellular energy production, muscle contraction, nerve impulse conductivity and proper bone mineralization, all of which are common health issues in the again male population.
BIO-ZINC 50 and BIO-ZINC/C CHEWABLE
Given that the body does not have a zinc reserve, zinc supplementation is vital for populations lacking sufficient zinc through dietary means, for those with absorption issues and in aging men. The benefits of a high potency zinc go far beyond hormone production, cellular metabolism, bone metabolism, spermatogenesis and longevity, given that it is required for over 300 enzymatic processes in the human body.
» Bio-Zinc 50
» Bio-Zinc/C Chewable Tablets
ADAPT-ADREN
An advanced adaptogenic herbal complex to protect against the physiologic complications associated with high levels of mental, physical and emotional stress. These herbs help to support the hypothalamic-pituitary-adrenal axis, with the pituitary gland being responsible for the initiation of hormone synthesis..
MITO-DETOX III
A unique blend of nutrients designed to aid in mitochondrial energy production, protect against oxidative stress, provide antioxidant support as well as support detoxification pathways.
» Mito-Detox III – 60 Caps size
» Mito-Detox III – 120 Caps size
References:
- Cleveland Clinic. Low Testosterone (Male Hypogonadism). Last reviewed 10 April 2018. Viewed 10 June 2020. https://my.clevelandclinic.org/health/diseases/15603-low-testosterone-male-hypogonadism
- Testosterone-What it Does and Doesn’t Do. Harvard Health Publishing. Harvard Medical School. Updated Aug 29 2019.
- Bachman E, et al. Testosterone Induces Erythrocytosis via Increased Erythropoietin and Suppressed Hepcidin: Evidence for a New Erythropoietin/Hemoglobin Set Point. J Gerontol A Biol Sci Med Sci. 2014 Jun; 69(6): 725–735.
- Langer C, Gansz B, Goepfert C, et al. Testosterone up-regulates scavenger receptor BI and stimulates cholesterol efflux from macrophages. Biochem Biophys Res Commun. 2002 Sep 6;296(5):1051-7.
- Guilliams T. Re-Assessing the Notion of “Pregnenolone Steal”. ZRT Laboratory Blog. Updated Wednesday, June 21, 2017. https://www.zrtlab.com/blog/archive/reassessing-pregnenolone-steal
- Abbott RD, Launer LJ, Rodriguez BL, et al. Serum estradiol and risk of stroke in elderly men. Neurology. 2007 Feb 20;68(8):563-8.
- Wranicz JK, Cygankiewicz I, Rosiak M, Kula P, Kareba W. The relationship between sex hormones and lipid profile in men with coronary artery disease. Int J Cardiol. 2005 May 11;101(1):105-10.
- Krieg M, Nass R, Tunn S. Effect of aging on endogenous level of 5 alpha-dihydrotestosterone, testosterone, estradiol, and estrone in epithelium and stroma of normal and hyperplastic human prostate. J Clin Endocrinol Metab. 1993 Aug;77(2):375-81
- Prins GS, Huang L, Birch L, Pu Y. The role of estrogens in normal and abnormal development of the prostate gland. Ann N Y Acad Sci. 2006 Nov;1089:1-13.
- Prins GS, Korach KS. The role of estrogens and estrogen receptors in normal prostate growth and disease. Steroids. 2008 Mar;73(3):233-44.
- Mellström D, Vandenput L, Mallmin H, et al. Older men with low serum estradiol and high serum SHBG have an increased risk of fractures. J Bone Miner Res. 2008 Oct;23(10):1552-60.
- Pernow Y, Hauge EM, Linder K, Dahl E, Sääf M. Bone histomorphometry in male idiopathic osteoporosis. Calcif Tissue Int. 2009 Jun;84(6):430-8.
- Jankowska EA, Rozentryt P, Ponikowska B. Circulating estradiol and mortality in men with systolic chronic heart failure. JAMA. 2009 May 13;301(18):1892-901.
- Langer C, Gansz B, Goepfert C, et al. Testosterone up-regulates scavenger receptor BI and stimulates cholesterol efflux from macrophages. Biochem Biophys Res Commun. 2002 Sep 6;296(5):1051-7.
- 10. Herbst KL, Amory JK, Brunzell JD, Chansky HA, Bremner WJ. Testosterone administration to men increases hepatic lipase activity and decreases HDL and LDL size in 3 wk. Am J Physiol Endocrinol Metab. 2003 Jun;284(6):E1112-8.
- Lerchbaum E, Pilz S, Boehm BO, Grammer TB, Obermayer-Pietsch B, März W. Combination of low free testosterone and low vitamin D predicts mortality in older men referred for coronary angiography. Clin Endocrinol (Oxf). 2012 Feb 22. doi: 10.1111/j.1365-2265.2012.04371.x.
- Lerchbaum, E., Trummer, C., Theiler-Schwetz, V. et al. Effects of vitamin D supplementation on androgens in men with low testosterone levels: a randomized controlled trial. Eur J Nutr 58, 3135–3146 (2019). https://doi-org.uws.idm.oclc.org/10.1007/s00394-018-1858-z
- Alwerdt J, Patterson AD, Sliwinski M. Gender Differences in Phytoestrogens and the Relationship with Speed of Processing in Older Adults: A Cross-Sectional Analysis of NHANES, 1999–2002. Nutrients. 2019 Aug; 11(8): 1780. Published online 2019 Aug 1. doi: 10.3390/nu11081780.
- Maggio M, De Vita F, Lauretani F, et al. The Interplay between Magnesium and Testosterone in Modulating Physical Function in Men. Int J Endocrinol. 2014;2014:525249. doi:10.1155/2014/525249
- Velarde MC. Mitochondrial and sex steroid hormone crosstalk during aging. Longev Healthspan. 2014; 3: 2. Published online 2014 Feb 5. doi: 10.1186/2046-2395-3-2
- Pitteloud N. et al. Relationship Between Testosterone Levels, Insulin Sensitivity, and Mitochondrial Function in Men. DIABETES CARE, VOLUME 28, NUMBER 7. JULY 2005
- Wang C, et al. Novel associations between sex hormones and diabetic vascular complications in men and postmenopausal women: a cross-sectional Study. Cardiovasc Diabetol (2019) 18:97 https://doi.org/10.1186/s12933-019-0901-6.
- Zhang S. et al. Endocrine disruptors of inhibiting testicular 3β-hydroxysteroid dehydrogenase. Chemico-Biological Interactions. April 2019; 303 (25):90-97.
- Schooling CM, Au Yeung SL, Freeman G, Cowling BJ. The effect of statins on testosterone in men and women, a systematic review and meta-analysis of randomized controlled trials. BMC Medicine. 2013; 11, 57. http://doi.org/10.1186/1741-7015-11-57.
- Chang CS, Choi JB, Kim H, & Park SB. Correlation between serum testosterone level and concentrations of copper and zinc in hair tissue. Biological Trace Element Research. 2011; 144(1-3), 264-271. doi:10.1007/s12011-011-9085-y.
- Malavolta M, Piacenza F, Basso A, Giacconi R, Costarelli L, Mocchegiani E. Serum copper to zinc ratio: Relationship with aging and health status. Mechanisms of Ageing and Development. November 2015; (151):93-100.
Medical Disclaimer: This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers/viewers of this content are advised to consult their doctors or qualified health professionals regarding specific health questions. Neither BioSpec Nutritionals, Practitioner Supply nor the publisher of this content takes responsibility for possible health consequences of any person or persons reading or following the information in this educational content. All viewers of this content, especially those taking prescription or over-the-counter medications, should consult their physicians before beginning any nutrition, supplement or lifestyle program.
Related Resources:
- Gonadal Steroidogenic Pathways INFOGRAPHIC, free download from BioSpec (pdf)
- Zinc INFOGRAPHIC, free download from BioSpec (pdf)