By Dr. Melissa Mitchell, DC, CFMP
The American Heart Association has existed since 1924, and since its inception has facilitated funding for groundbreaking research and heart health awareness based on the efforts of doctors, researchers and volunteers.¹ Despite their best efforts, heart disease remains the number one cause of death not only in the US, but worldwide. This continuing trend would indicate that perhaps there remain aspects of the cardiovascular disease matrix that have not been addressed sufficiently and/or limited and misinformation perseveres in the medical community.
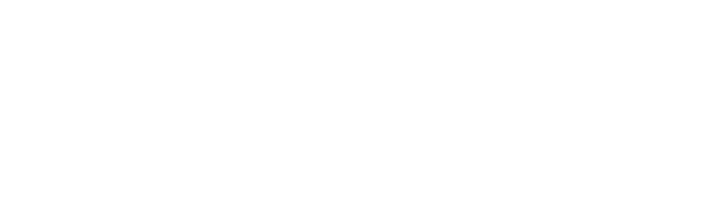
Cardiovascular disease is a general term that includes any disease process affecting the heart and/or blood vessels. The likelihood of someone developing cardiovascular disease is largely the result of modifiable lifestyle behaviors and/or physiological risk factors.²
Behavioral and Physiological Risk Factors for Cardiovascular Disease
Cholesterol, the Scapegoat
Cholesterol and other dietary fats continue to be unfairly stigmatized in mainstream medicine, a pattern that has lasted for over half a century in part based on research by Ancel Keys. Keys promoted the idea that consumption of dietary fats (and particularly those from animal sources) were largely responsible for the dramatic rise in rates of cardiovascular disease. Though Keys personally supported eating patterns more aligned with a Mediterranean style diet, consisting largely of polyunsaturated fats, the trend favoring low-fat diets continued throughout the 1980’s and 90’s in favor of the narrative that calorie-dense fats (at 9 calories per gram vs 4 calories in carbohydrates and protein) led to greater rates of obesity and cardiovascular disease. This trend was further bolstered by funding and manipulation from the sugar industry, which worked to conceal their role in the alarming rise of cardiovascular disease while deflecting blame in the direction of dietary fats.
To capitalize on this low-fat trend, many food manufacturers replaced the flavor-enriching properties of fat with sugar and sugar substitutes, an initiative that would widen the floodgates of metabolic dysfunction and cardiovascular disease in the years that followed. Yet despite increasing disease rates, many healthcare professionals remained unaware or unconvinced of the damage caused by popular low-fat diets as refined carbohydrates and processed foods had become a mainstay of the Standard American Diet (SAD). Fortunately, more recent research is supportive of the notion that most dietary fats, including cholesterol, do not influence blood lipids and cardiovascular disease to the degree once thought.³, ⁵ The same cannot be said for trans fats and sugar, both of which contribute significantly to unhealthy blood lipids and cardiovascular disease risk.
Blood Lipids and their Functions
Cholesterol is a waxy lipid (fat) synthesized in the liver and found in all cells and plasma. It is a vital component of cell membranes that serves to stabilize and maintain the fluidity of the cell, it allows for transport of molecules across the cell membrane, and is involved in cellular communication and nerve conduction. Cholesterol is also an essential precursor of various steroid hormones, bile, and vitamin D synthesis.⁴
Triglycerides are the most common form of fat in food and the body, consisting of three fatty acids attached to a glycerol molecule. Following digestion, absorption, and processing in the liver for transport, triglycerides are broken down by lipoprotein lipase to facilitate free fatty acid entry into adipocytes (fat cells) where they are subsequently re-formed for storage. While adipocytes provide the main storage reservoir for triglycerides, other sites include the liver, skeletal muscle, and blood (to a smaller degree). Triglycerides fulfill the primary role as the most abundant energy reserve in the body, which can be utilized by cells during times of increased demand (such as exercise) or when energy from food is in limited supply.⁴
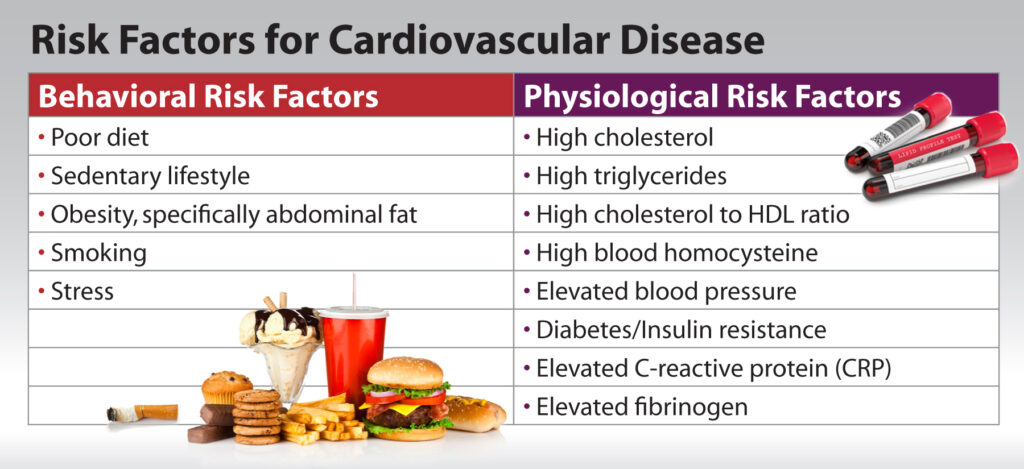
It is necessary to understand that fats (whether from foods or mobilized from body stores) cannot be transported freely in the blood given their inability to mix well with water, and thus require the assistance of protein transporters. Lipoproteins perform this function by moving cholesterol and triglycerides to various tissues for utilization in a wide range of physiological processes.
There are several types of lipoproteins, which are classified largely based on the contents they transport. The most readily identified lipoproteins, particularly in the context of cardiovascular disease, include: low density lipoproteins (LDL), very low density lipoproteins (VLDL), and high density lipoproteins (HDL). Aside from their role in triglyceride and cholesterol transport, lipoproteins are involved in other biological processes including coagulation and tissue repair, and can serve as carriers for a number of hydrophobic compounds. Among the primary classes identified, lipoproteins can be further subdivided into classifications that vary in size and density that carry additional associations with the risk and progression of cardiovascular disease. Other Lipoproteins that are not routinely tested are IDL and Lipoprotein(a) [Lp(a)], the latter of which is extremely telling of cardiovascular disease risk. ⁶
Among lipoproteins, HDL is the smallest and most dense and has been revered as the “good cholesterol” because of its role in scavenging cholesterol throughout the body (especially the arterial walls) for transport back to the liver for elimination. LDL and VLDL on the other hand are larger in size and less dense compared to HDL. These lipoproteins perform the necessary role of distributing cholesterol throughout the body for utilization among cells. Within the bloodstream, LDL particles can easily become wedged within damaged endothelial (arterial) lining and promote the development of plaque accumulation (atherosclerosis), hence the reason it is labelled the “bad cholesterol.” ⁶
Blood Lipids Testing
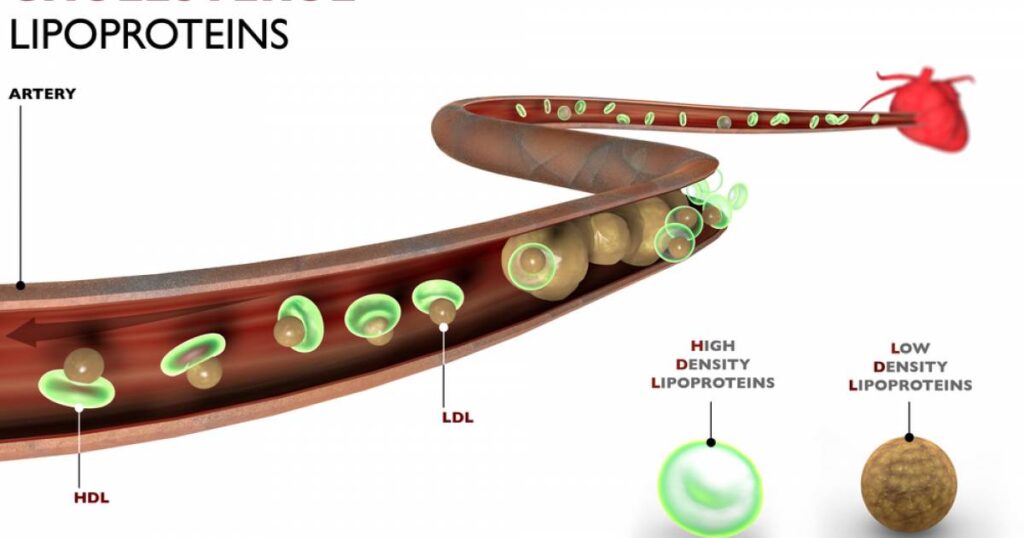
Many institutions, along with the American Heart Association, only promote routine testing of total cholesterol, HDL, LDL and VLDL. However, more recent research has served to expose the limitations of these tests for assessing true cardiovascular disease risk. For instance, additional considerations are available to distinguish lipoprotein profile from within a larger classification. Consider LDL particles for example, which classically are evaluated as homogenous in terms of their presentation and level of cardiovascular risk when elevated. However, LDL particles may further be distinguished based on the observation that smaller dense particles (among other LDL particles) are more prone to remain within the bloodstream, are more readily oxidized, and are more likely to become lodged within damaged vessel walls. Thus, different patients may have the same LDL cholesterol values, but atherosclerosis risk will be greater (assuming all other risk factors are identical) in the patient with less favorable LDL particle size. For this reason, it is imperative that routine blood lipid panels include lipoprotein particle size to pinpoint those at higher risk of a life-threatening cardiovascular event.
LDL particle size/density and quantity determine risk, which is not tested for in routine cholesterol bloodwork.
Other Informative Tests
Aside from traditional blood lipid panels, other tests are essential based on their strong association with cardiovascular disease. A common underlying factor in heart disease is long term blood sugar dysregulation/diabetes, thus making it imperative to include fasting glucose, fasting insulin and hemoglobin A1c (Hb A1c). Systemic inflammation is also a primary concern in the progression of cardiovascular disease. As such, high sensitivity C-Reactive Protein (hsCRP) and homocysteine must also be evaluated. For those who remain at elevated risk of cardiovascular disease, running these tests routinely (in addition to blood lipid panels) allows for a more robust evaluation of treatment efficacy (especially pharmacological, diet, and lifestyle), which in turn will result in better long-term health outcomes.
Reference and Optimal Range
In medicine it is well-accepted that chronic disease progresses gradually over a period of time along a continuum, and is generally not consistent with a sharp dichotomy that signifies ‘disease’ (or lack thereof) once a lab value falls outside of the ‘normal’ reference range. The continuum of disease and health in a patient can be monitored through close evaluation of valid symptoms combined with laboratory analysis by which a steady progression (or remission) of physiological risk factors are observed. Many traditional practitioners only address lab values after they’ve fallen outside of the ‘normal’ range, thus ignoring patient symptoms that may appear along the steady path of decline, yet remaining within an acceptable (normal) range.
Fortunately, many diligent healthcare practitioners are beginning to look at ‘optimal’ lab values with a more refined range, and based on more recent research, to address early trends and take a more proactive approach in the health of their patients. Disease, or increased risk of disease, is much easier to address when identified early and correctly based on appropriate diagnostics and their reference ranges.
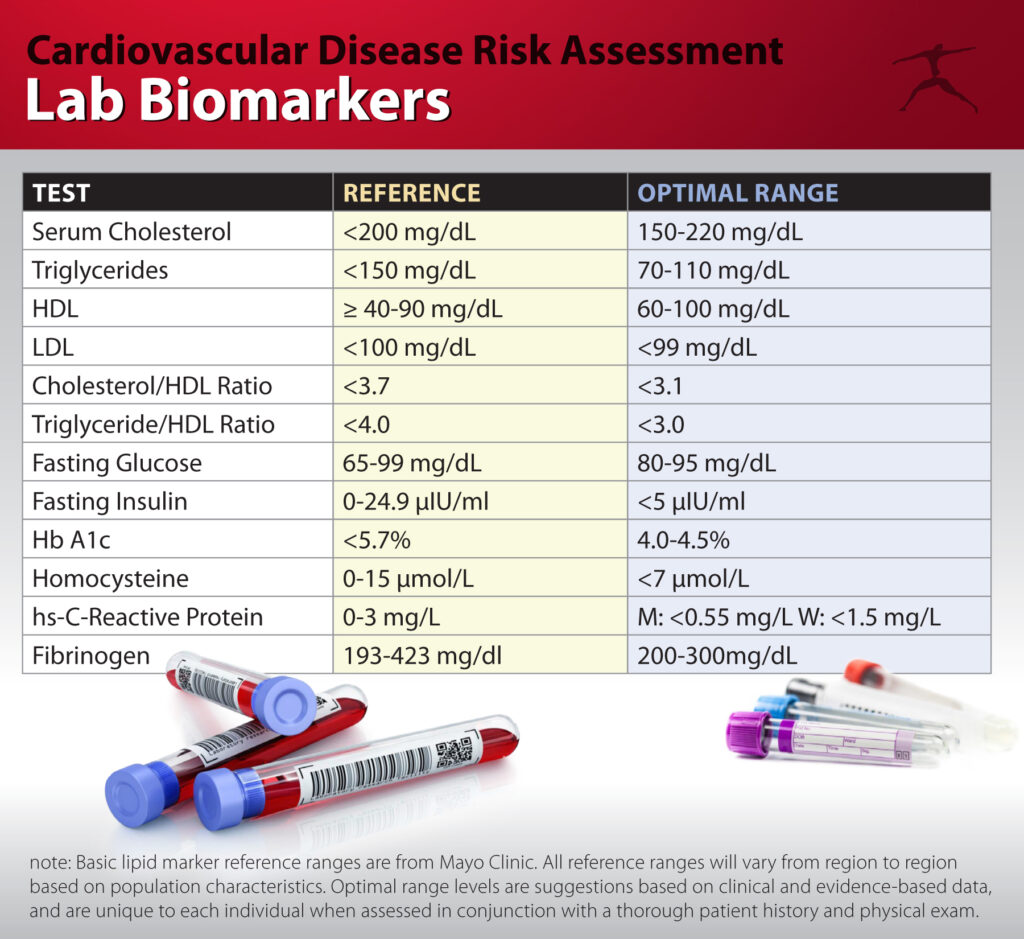
Lab biomarkers for traditional cholesterol lipid profile, and additional tests.
When assessing cardiovascular disease risk in a patient, it is crucial that practitioners (and health insurance companies) expand their testing beyond basic lipid profile panels. Additional lipoprotein tests, along with inflammatory and blood sugar markers, would be much more telling and valuable when monitored routinely to further understand those who are truly at greater risk. These tests would serve to justify the necessity and extent of lifestyle and pharmaceutical interventions for the individual patient rather than basing health decisions on limited data and recommendations for the general population.
References:
- American Heart Association. Our Lifesaving History. Viewed Feb 10, 2020. https://www.heart.org/en/about-us/history-of-the-american-heart-association
- American Heart Association. Understand your risks to prevent a heart attack. Viewed Feb 10, 2020. https://www.heart.org/en/health-topics/heart-attack/understand-your-risks-to-prevent-a-heart-attack
- Soliman, G. Dietary Cholesterol and the Lack of Evidence in Cardiovascular Disease. Nutrients. 2018 Jun; 10(6): 780. Published online 2018 Jun 16.
- Blood Cholesterol, Blood Lipids and Heart Health. University Health Service. University of Michigan. Viewed Feb 10, 2020. https://www.uhs.umich.edu/cholesterol
- Mozaffarian, D., Ludwig, D. S., “The 2015 US Dietary Guidelines-Lifting the Ban on Total Dietary Fat” Journal of the American Medical Association. June 23/30. Volume 313, Number 24.
- Feingold, K. R., Grunfeld, C. Introduction to Lipids and Lipoproteins. [Updated 2018 Feb 2]. In: Feingold, K. R., Anawalt, B., Boyce, A. et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK305896/
Medical Disclaimer: This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of such advice or treatment from a personal physician. All readers/viewers of this content are advised to consult their doctors or qualified health professionals regarding specific health questions. Neither BioSpec Nutritionals, Practitioner Supply nor the publisher of this content takes responsibility for possible health consequences of any person or persons reading or following the information in this educational content. All viewers of this content, especially those taking prescription or over-the-counter medications, should consult their physicians before beginning any nutrition, supplement or lifestyle program.