April – IBS Awareness Month
By Dr. Melissa Mitchell, DC, CFMP
News & Science Behind Formulas, Discounts & Offers, Resources & Links
As April comes to a close, so does the observation of IBS month. The estimated 10-15% of adults in the US who suffer from IBS symptoms, however, will continue to live with the symptoms every day. In support of IBS Awareness Month, the educational information below provides an overview and strategies to help address this common GI health condition.
WHAT IS IBS?
Irritable Bowel Syndrome (IBS) is a condition in which the gastrointestinal system loses functionality and is associated with abdominal pain and change in bowel habits.¹
SIGNS AND SYMPTOMS ¹
- Abdominal pain
- Bloating/Abdominal distention
- Excessive flatulence
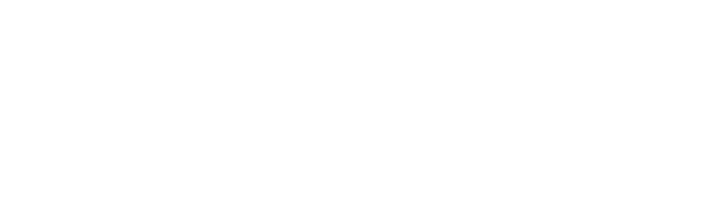
- Diarrhea that can be accompanied with urgency (>3 bowel movements/day)
- Constipation what can be associated with excessive strain (<3 bowel movements/week)
ETIOLOGY
It remains unclear as to the specific etiology of IBS, but contributing factors have been established based on clinical and epidemiological research.²
Low-Grade Inflammation – Patients with IBS show increased values of inflammatory markers upon testing although colonic biopsies do not reveal any visible inflammation. ³·⁴
Altered Motility – Those that suffer with constipation have significantly slower motility in combination with reduced gastrointestinal contractions⁵ and altered passage of intestinal gas.⁶
Alteration of Intestinal Microbes (Dysbiosis) – IBS patients have gastrointestinal microbiota that differ from those without IBS, showing lower levels of beneficial bifidobacteria and lactobacilli species and harmful levels of enterobacteriaceae.⁷·⁸·⁹
Heightened Perception – It has been found that people with IBS have increased intestinal sensitivity to painful stimuli. ³·¹º In response to a triggering event such as inflammation, stress, or trauma, the gut can become sensitized to luminal distension, resulting invisceral hypersensitivity. Furthermore, hypersensitivity in IBS patients is not just limited to the gut, and more widespread alterations in central pain processing may be involved in this chronic pain disorder.
POSSIBLE RISK FACTORS
Genetic predisposition – The predisposition is not specific to IBS but rather the reaction of the central nervous system in response to stimuli and stress. Individuals more susceptible to the effects of stress have a greater tendency to develop IBS.¹¹
Gastrointestinal Infections – Alteration of the microbiome in response to an infection sets the stage for chronic alterations in both gastrointestinal structure and function related to the onset of IBS.¹²·¹³
Antibiotic Use – It has been suggested that alterations in the gut microflora following antibiotic use contributes to the development of IBS and amplified visceral perception.¹⁴
Stress/Trauma – The onset of IBS can follow a stressful or traumatic life event¹⁵ and these patients may also present with other psychiatric conditions such as anxiety and depression.¹⁶
IBS DIAGNOSIS
Diagnosis of IBS is a diagnosis of exclusion, meaning that there is an absence of any other gastrointestinal pathology in combination with the lack of any biological markers or diagnostic testing to confirm IBS.¹⁷ As such, the Rome IV Criteria is used to diagnose IBS.
Rome IV Criteria ¹⁸
Recurrent abdominal pain at least 1 day per week in the last 3 months with the onset of initial symptom(s) for at least 6 months, associated with 2 or more of the following:
- Related to defecation
- Associated with a change in stool frequency
- Associated with a change in appearance of stool
SUBTYPES OF IBS RELATED TO SYMPTOMATOLOGY ¹⁸
- Constipation-predominant (C-IBS)
- Diarrhea-predominant (D-IBS)
- Mixed IBS (M-IBS)
- Untyped IBS (presents with abdominal pain with no change in stool frequency and form)
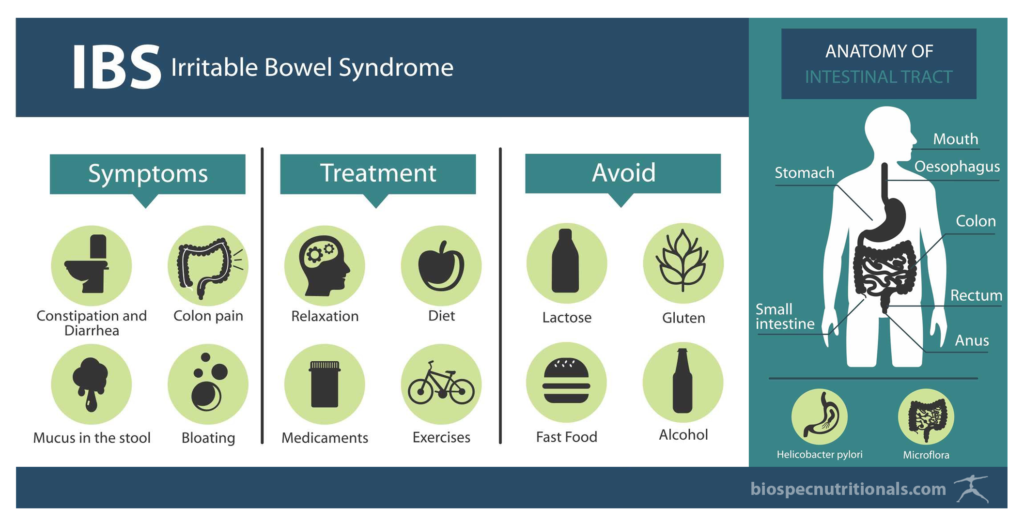
The Whole Systems Approach to IBS
There are a number of pharmaceutical agents that are utilized to treat patients suffering with IBS that have lacked in their efficacy for many patients and oftentimes have severe side effects.¹⁹ A more holistic approach is necessary to address the factors that may contribute to one’s gastrointestinal dysfunction.
KEYS TO ADDRESSING IBS
1) Enhance the gut microflora.
Introduce more beneficial bifidobacterium and lactobacilli species²º through supplementation and fermented foods as well as utilizing prebiotics to feed beneficial gut bacteria, specifically galactooligosaccharides (GOS).²¹
2) Address small intestinal bacterial overgrowth (SIBO), if applicable.
Eliminate harmful bacteria with the use of probiotics and herbal formulas.²² Consider antimicrobial herbal therapies that can selectively remove harmful bacteria species. Fresh garlic (3 – 4 gloves per day), pomegranate rind, and green tea polyphenols are among the most effective antimicrobial foods.
3) Implement therapeutics and lifestyle changes.
Promote more frequent, healthy bowel movements in C-IBS with fibre, fluids and daily moderate exercise.²³·²⁴
- Ways to increase fiber intake: ground flax seed, slippery elm, psyllium husk, chia seeds, oat bran, pectin, leafy green salads, beetroot, ≥4 servings of fruit/day (kiwi and blackberries specifically).
- Body Weight ÷ 2 = ounces of water per day.
Increase water intake with perspiration and increased levels of activity.
4) Manage symptoms associated with IBS.
Address constipation, diarrhea, gas, nausea with supplements and/or herbal formulas.
5) Decrease gastrointestinal inflammation and hypersensitivity.
Incorporate specific herbs and other therapeutics.
- Herbs: turmeric, licorice root, ginger, chamomile and peppermint in combination with caraway²⁵
- Other therapeutics: melatonin has shown to decrease GI sensitivity²⁶
6) Support a robust nervous system.
Allow for a proper gastrointestinal response to stimuli.
- Chiropractic care²⁷: restore proper function of the Vagus Nerve, allowing the nervous system to send proper signals to the digestive system
- Adaptogenic herbs: Schisandra chinensis, Rhodiola rosea, Panax ginseng
- Incorporate stress management techniques: yoga, meditation, and other mindful practices – all of which are well-supported for their mitigating effects on stress, with other evidence supporting a positive effect on pain sensitization of the central and peripheral nervous systems.
7) Support healthy liver function
Poor liver function is often viewed as an important contributing factor in IBS, with liver congestion as a cause of constipation. Consider therapeutics including turmeric, globe artichoke, milk thistle and/or dandelion root.
8) Address food allergens and intolerances
Consider dietary changes based on food trials, utilizing a journal or app.
- Elimination Diet » UW Integrative Health: The Elimination Diet (pdf)
- Low FODMAPs Diet » UW Integrative Health: The FODMaP Diet (pdf)
- Eliminate gluten » UW Integrative Health: Gluten-Free Diet guidance
THE CASE FOR PROBIOTICS: IBS AND BEYOND
Humans have been consuming probiotics for thousands of years, yet the potential for probiotics in human health is just beginning to be recognized at a widespread level. Probiotics are often depicted and described in various ways based on a particular context or sphere of influence, yet it’s essential to understand probiotics for what they truly are in the biological sense – ‘live microorganisms which when administered in adequate amounts confer a health benefit on the host’. While probiotic research over the past 20 years has led to exponential gains in determining distinct species characteristics and clinical applications, probiotic microorganisms have always been an important component of the human diet and health.
Strain Specificity: The Most Critical Consideration
Probiotics are readily obtained through fermented foods or as dietary supplements, which can vary dramatically based on their characteristics and benefits to the host. Probiotics are classified according to genus, species, and strain, with probiotics of the same genus (e.g. Lactobacillus, Bifidobacterium, Saccharomyces) and strain (e.g. Lactobacillus plantarum, Lactobacillus rhamnosus, Lactobacillus acidophilus) often sharing common properties. However, the absolute most important consideration when selecting probiotics for clinical use is STRAIN SPECIFICITY, which refers to the unique designation that differentiates individual strains within the same probiotic genus/species classification.
Considering that many commercial probiotic strains may belong to the same species, such as Lactobacillus rhamnosus for example, one may reasonably assume that all probiotic strains belonging to this species produce a similar outcome on the host. This is NOT the case! The uniqueness of an individual strain within the same species, as identified by the strain designation, such as GG or CNCM I-3690 within the Lactobacillus rhamnosus genus/species for example, can be likened to different breeds of dogs. Sure, all dogs belong to the same species and often express similar behaviors, yet they differ tremendously between breeds in terms of size, appearance, strength, and purpose. Clearly, it should not be assumed that a pug could fulfill the herding responsibilities of a border collie, right? The same is true of distinct probiotic strains.
Essentially, when determining the likelihood of whether a particular probiotic formula, which will typically include a combination of different strains, is likely to benefit a particular condition, whether IBS or non-gastrointestinal related, one must look primarily to the research supporting the efficacy of a strain in relation to the condition at hand.
Determining the Correct Probiotic Formula
Though the specific biological mechanisms by which probiotics serve to benefit the human host are beyond the current discussion, the essential takeaways at this time (from information presented) are that probiotic formulas should be selected based upon the efficacy of individual strains included in the formula, which should ideally be supported by clinical trials in humans. The following points may be considered when selecting a specific probiotic formula:
- Dosage – While minimum effective dosages appear to differ by strain, most successful probiotic research has utilized strains >10^9 CFU/dose. This minimum amount should be present for each strain in a formula.
- Safety – Clinical studies should be available to show that all included strains are safe for human consumption, with specific subpopulations identified when consumption may pose a risk (e.g. younger children, immune compromised, etc.)
- Colonization – Though probiotic supplements do not permanently colonize the gastrointestinal tract, they should be able to adhere to the intestinal mucosa and serve as temporary residents while supporting the proliferation of more permanent bacteria communities.
- Clinical Efficacy – Documented clinical evidence should be available to support the use of a specific probiotic strain in relation to a specific condition or general health claim (e.g. increased immune activity, lactose digestion, etc.). Again, clinical efficacy is a matter of strain specificity.
As an excellent resource for selecting the correct probiotic formula for a given condition, based on clinical research, please visit Probiotic Advisor – www.probioticadvisor.com
References
- American Gastroenterology Association. Irritable bowel syndrome: a technical review for practice guideline development. Gastroenterology 2002: 112:2120-2137.
- Mayer EA. Emerging disease model for functional gastrointestinal disorders. AM J Med 1999; 107(5A):125-195.
- Camilleri M, et al. Consensus report: clinical perspectives, mechanisms, diagnosis and management of irritable bowel syndrome. Aliment Parmacol Ther 2002;16:1407-1430.
- Berick P, et al. Is irritable bowel syndrome a low-grade inflammatory bowel disease? Gastroenterol Clin North Am. 2005;34:235-245
- Coulie B, Role of GI motor abnormalities in irritable bowel syndrome. ACta Gastroenterol Belg. 2001;64:276-280.
- Serra J, et al. Impaired transit and tolerance of intestinal gas in irritable bowel syndrome. Gut 2001;48:14-19.
- Si JM, et al. Intestinal microecology and quality of life in irritable bowel syndrome patients. World J Gastroenterol 2005;10:1802-1805.
- Manlinen E, et al. Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR. Am J Gastroenterol. 2005;100:373-382.
- Balsari A, et al. The fecal microbial population in the irritable bowel syndrome. Microbiologica. 1982;5:185-194.
- Delavaux M. Role of visceral sensitivity in the pathophysiology of irritable bowel syndrome. Gut 2002;51(suppl. 1):i67-i71.
- Morris-Yates AD, et al. Evidence of a genetic contribution to self reported symptoms of irritable bowel syndrome. Gastroenterol. 1995;108:A652.
- Rodriguez LAG, Ruigomez A. Increased risk of irritable bowel syndrome after bacterial gastroenteritis: cohort study. BMJ. 1999;318:565-566.
- Gwee KA, et al. The role of psychological and biological factors in postinfective gut dysfunction. Gut. 1999;44:400-406.
- Maxwell PR, et al. Antibiotics increase functional abdominal symptoms. Am J Gastroenterol. 2002;97:104-108.
- Whitehead WE, etal. Symptoms of psychological distress associated with irritable bowel syndrome. Gastroenterol. 1998;95:709-714.
- Hichstrasser B, Angst J. The Zurich study. XXII. Epidemiology of gastrointestinal complaints and comorbidity with anxiety and depression. Eur Arch Psychiatry Clin Neurosci. 1996;246:261-272.
- Schmulson MW, Chang L. Diagnostic approach to the patient with irritable bowel syndrome. Am J of Med. 1999;107:5:20-26.
- Lacy B, Patel N, Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J Clin Med. 2017; 6(11):99.
- Schoenfeld P. Efficacy of current drug therapies in irritable bowel syndrome: what works and does not work. Gastroenterol Clin N Am 2005;34:319-335.
- Gibson GR, Roberfroid MB. DIetary modulation of the human colonic microbiota: introducing the concept of prebiotics. J Nutr 1995;125:1401-1412.
- Silk DBA, et al. Clinical trial: the effects of a trans-galactooligosaccharide prebiotic on faecal microbiota and symptoms in irritable bowel syndrome. Aliment Pharmacol Ther. 2009; 29:508-518.
- Ford AC, Spiegel BM, Talley NJ, Moayyedi P. Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2009;7:1279–1286.
- Sanjoaquin MA, et al. Nutrition and lifestyle in relation to bowel movement frequency: a cross-sectional study of 10,630 men and women in EPIC-Oxford. Public Health Nutr 2004;7:77-83.
- Everhart JE, et al. A longitudinal survey of self-reported bowel habits in the United States. Dig Dis Sci. 1989;34:1153-1162.
- Adam B, et al. A combination of peppermint oil and caraway oil attenuates the post-inflammatory visceral hyperalgesia in a rat model. Scand J Gastroenterol. 2006;41(2);155-60.
- Lu WZ, Gwee KA, Moochhalla S, Ho KY. Melatonin improves bowel symptoms in female patients with irritable bowel syndrome: a double-blind placebo-controlled study. Aliment Pharmacol Ther. 2005;22:927–934.
- Welch A, Boone R. Sympathetic and parasympathetic responses to specific diversified adjustments to chiropractic vertebral subluxations of the cervical and thoracic spine. J Chiropr Med. 2008 Sep;7(3):86-93.
SUMMARY
- Consider etiology and risk factors, root causes for IBS symptoms
- Enhance the gut microflora
- If applicable, address small intestinal bacterial overgrowth (SIBO)
- Implement therapeutics and lifestyle changes: increase fiber intake, and more water with exercise and perspiration
- Manage IBS symptoms with supplements and/or herbal formulas
- Decrease GI inflammation and hypersensitivity with herbs and therapeutics
- Support the nervous system with chiropractic care, adaptogenic herbs, and stress management techniques
- Support healthy liver function
- Address food allergens and intolerances
related off-site resources (not affiliated with BioSpec)
The Elimination Diet (pdf)
The FODMaP Diet (pdf)
Gluten-Free Diet Guidance (uwhealth.org)
Probiotics for IBS and SIBO, with Dr. Hawrelak (video)
probioticadvisor.com (Dr. Hawrelak’s website)
Resources & LinksBioSpec Nutritionals is not affiliated or endorsed by any of the organizations related to off-site links shared in this newsletter
May 2020 Discount Offer
— PRODUCTS FOR IBS —

Specific Formulas for GI Support
____________
Ultra-Biotic 50
The highest potency probiotic from BioSpec contains 50 billion CFUs per serving,
with 12 diverse strains of the Lactobacilli and Bifidobacteria genera.
Probiotic-5
A robust probiotic formula provides 5 billions CFUs per servicing, with 5 of the most robust, well-documented bacteria strains identified to support digestive, intestinal, and immune health.*
Gastri-Ease HP
A potent blend of nutrients and herbal extracts with GI specific antimicrobial and mucosal healing properties.*
Inflam-95
Help reduce systemic inflammation with clinical levels of Ayurvedic Herbs, with additional ingredients to support digestive, liver, kidney and connective tissues*.
____________
— ONGOING OFFERS —

Free Shipping
Get FREE shipping when you shop online.
Applies to all retail and wholesale orders.
No minimums. No code needed.
— PRACTITIONER OFFERS —

Free Brochures, Samples, and other B2B Benefits
- FREE educational brochures (bundled), shipped free of charge
- FREE product samples available, including CBD products
- FREE price lists and other B2B support, as part of BioSpec Practitioner Programs
Contact us to fulfill your request.
Some limits and restrictions may apply.
Medical Disclaimer: This content is for informational and educational purposes only. It is not intended to provide medical advice or take the place of such advice or treatment from a personal physician. All readers/viewers of this content are advised to consult their doctor or qualified health professional regarding specific health questions. Neither BioSpec Nutritionals, Practitioner Supply nor the publisher of this content takes responsibility for possible health consequences of anyone reading or following the information in this educational content. All viewers of this content, especially those taking prescription or over-the-counter medications, should consult their physicians before beginning any nutrition, supplement or lifestyle program.