Glaucoma is a leading cause of irreversible blindness around the world. The most common form of glaucoma in the US and worldwide is age related, open-angle glaucoma, which is the form most typically identified when discussing the disease.1 Over time, a buildup of pressure within the eye damages the optic nerve causing peripheral blindness initially, which can later progress to total blindness if left untreated.² One in three people with open-angle glaucoma experience normal-tension glaucoma, where damage to the optic nerve occurs in the absence of eye pressure. In infancy, congenital glaucoma prevents normal drainage of the eye and creates increased pressure, causing damage to the optic nerve. Other forms of glaucoma that are not congenital may also occur in children and are labeled pediatric glaucoma. A more serious form of glaucoma, angle-closure glaucoma, can present with intense eye pain, blurred vision, nausea and redness of the eye. This is a medical emergency and should be treated immediately. There are also secondary glaucomas that can occur as a result of other conditions such as diabetes and elevated blood pressure.³
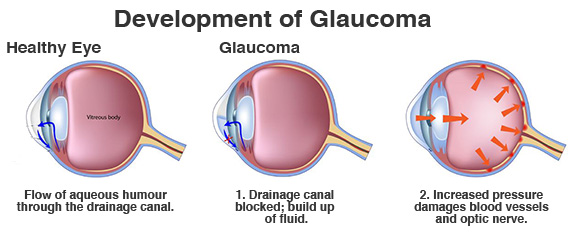
Glaucoma Diagram: Fluid buildup in the eye increases pressure, called intraocular pressure, and can damage the optic nerve. The most common type of glaucoma (open-angle glaucoma) often has no symptoms other than slow vision loss.
Generally speaking, there are no early signs or symptoms associated with open-angle glaucoma, and thus many remain unaware of their risk until the later stages of disease. Increased risk for developing open-angle glaucoma is more likely in adults over 60, African American or Hispanics over 40, diabetics, and those with a family history of the disease. Regarding normal-tension glaucoma, greater risk is associated with a family history of disease, being of Japanese descent, and the presence of cardiovascular conditions including arrhythmias and low blood pressure.²⁻⁴
There remains limited understanding as to the causes of increased intraocular pressure and decreased fluid drainage within the eye, the most significant factors behind open-angle glaucoma. Although a universal standard for prevention has yet to be recognised, early detection by dilated eye examination remains the best preventative approach. Existing treatments can involve medication, laser therapy, or surgery, yet glaucoma tends to progress in many individuals despite sustained intervention or the absence of increased intraocular pressure. Considering the current deficit of available knowledge, as well as the shortcomings of existing treatments, it’s prudent to recognize the influence of other unidentified risk factors and potential strategies to mitigate their impact.
studies and clinical trials suggest a link between antioxidant status and risk for prevalent glaucoma
A recent review of current research examining a series of epidemiological studies and clinical trials suggest a link between antioxidant status and risk for prevalent glaucoma.1 As with most degenerative conditions associated with aging, an imbalance between reactive oxygen species (ROS) and antioxidants is thought to play a fundamental role. Specific to glaucoma pathophysiology, oxidative stress may contribute to glaucoma by damaging the cells in the trabecular meshwork, thus interfering with normal drainage of aqueous humor and increasing intraocular pressure.1 Oxidative stress may also contribute directly to the death of retinal ganglion cells of the inner retina by damaging mitochondrial networks essential for cellular function and survival.1 The mechanisms by which oxidative imbalances can manifest and contribute to glaucoma progression and severity are complex and lack decisive conclusion. However, considering the protective role of antioxidants for combating oxidative stress and mitochondrial dysfunction, it is reasonable to consider specific nutritional approaches to support those at increased risk for developing glaucoma, or to potentially augment primary treatments in existing patients.
In relation to retinal health and long-term risk for age-related eye disease, lutein and zeaxanthin are unique among other carotenoids due to their ability to cross the blood-retinal barrier and exert strong antioxidant activity.5 While available data remains inconclusive based on clinical trials involving glaucoma patients – largely a consequence of inconsistencies in study design and measurement techniques between studies – a strong rationale remains for lutein and zeaxanthin as a complementary approach among glaucoma patients or those at increased risk, especially when considering their excellent safety profile, reasonable cost, and well-documented molecular activities supporting vision health.1 Of course, more comprehensive clinical trials must be conducted before specific treatment recommendations should be made among patients with glaucoma.

Vision-Plex by BioSpec Nutritionals is an antioxidant carotenoid complex containing lutein and zeaxanthin, which is designed to support visual function through increased antioxidant status within the cells of the retina.*
References:
- Lawler T, Liu Y, Christensen K, Vajaranant TS, Mares J. Dietary Antioxidants, Macular Pigment, and Glaucomatous Neurodegeneration: A Review of the Evidence. Nutrients. 2019 May; 11(5): 1002.
- National Eye Institute. (2019). Glaucoma. National Institute of Health.
- National Eye Institute. (2019). Types of Glaucoma. National Institute of Health.
- Glaucoma Research Foundation. (October 29, 2017). Glaucoma Facts and Stats.
- Bhosale P., Larson A.J., Frederick J.M., Southwick K., Thulin C.D., Bernstein P.S. Identification and characterization of a Pi isoform of glutathione S-transferase (GSTP1) as a zeaxanthin-binding protein in the macula of the human eye. Journal of Biological Chemistry. 2004;279:49447–49454.
Medical Disclaimer: This content is for informational and educational purposes only. It is not intended to provide medical advice or take the place of such advice or treatment from a personal physician. All readers/viewers of this content are advised to consult their doctor or qualified health professional regarding specific health questions. Neither BioSpec Nutritionals, Practitioner Supply nor the publisher of this content takes responsibility for possible health consequences of anyone reading or following the information in this educational content. All viewers of this content, especially those taking prescription or over-the-counter medications, should consult their physicians before beginning any nutrition, supplement or lifestyle program.
*The above statements have not been evaluated by the Food and Drug Administration These products are not intended to diagnose, treat, cure or prevent disease.